- Case report
- Open access
- Published:
A 14-year-old boy with multiple trauma and bilateral basal ganglia hemorrhage due to coronavirus disease 2019: a case report
Journal of Medical Case Reports volume 17, Article number: 88 (2023)
Abstract
Background
In December 2019, coronavirus disease 2019 spread worldwide, causing acute respiratory distress syndrome. Coronavirus disease 2019 presents from an asymptomatic infection to severe disease causing multiorgan failure. Neurological manifestations were observed in some patients, including intracerebral hemorrhage. Bilateral basal ganglia hemorrhage is rare due to trauma.
Case presentation
Our patient was a 14-year-old Iranian boy with multiple trauma and loss of consciousness who tested positive for coronavirus disease 2019. The brain computed tomography scan reported bilateral basal ganglia hemorrhage. Bilateral ground glass opacity was reported through a chest computed tomography scan.
Discussion and conclusions
In this study, we reported a 14-year-old boy referred to the emergency room due to multiple trauma. Through the medical interventions, bilateral basal ganglia hemorrhage was discovered incidentally. Coronavirus disease 2019 was detected in this patient on the basis of findings in chest computed tomography scan and positive real reverse transcription polymerase chain reaction test. Several clinical reports and series exploring the relationship between coronavirus disease 2019 and ischemic strokes have been published. Coronavirus disease 2019, like other acute respiratory syndromes, can invade the central nervous system through hematogenous and neuronal dissemination or it can be an immune response to the cytokine storm. In conclusion, it is vital to know the pathophysiology of the neurological manifestations of coronavirus disease 2019 and prevent the mild neurological manifestations leading to severe conditions.
Introduction
Severe acute respiratory syndrome–coronavirus-2 (SARS–CoV-2) caused coronavirus disease 2019 (COVID-19) in Wuhan, China in December 2019. COVID-19 is a contagious respiratory disease spreading worldwide [1]. COVID-19 can appear from an asymptomatic situation to acute respiratory distress syndrome (ARDS) and eventually multiorgan damage [2]. The central nervous system (CNS) can be involved in COVID-19. Some neurological manifestations of COVID-19 include dizziness, headache, hypogeusia, hyposmia, ataxia, seizure, ischemic stroke, cerebral hemorrhage, encephalopathy, encephalitis, meningitis, seizure, cerebral vein thrombosis, and Guillain–Barre syndrome [3]. Intracranial hemorrhage (ICH) is an uncommon situation due to COVID-19. This may happen because of some risk factors such as arterial hypertension or anticoagulant therapy [2]. Expression of angiotensin-converting enzyme 2 (ACE2) in glial cells and neurons may be a possible etiology for the neurological manifestation of COVID-19 [4]. In this case study, we will report bilateral basal ganglia hemorrhage in a 14-year-old boy who tested positive for COVID-19 and denied any past medical history or anticoagulant consumption.
Case presentation
The case is a 14-year-old Iranian boy with no past medical history presenting with multiple trauma from a motorcycle accident who was transferred to the Poursina hospital emergency room (ER) in Rasht on 9 June 2020. In addition, he had an extensive laceration on his right knee and a star-shaped laceration on his parietal region. O2 saturation was 93%, temperature was 38.5 °C, and the other vital signs were stable. In the ER, his Glasgow Coma Scale (GCS) score was 3/15 (E1V1M1). No free fluid in the abdomen and pelvic cavity in focused assessment with sonography for trauma was reported. A right bundle branch block was observed in his electrocardiogram (ECG). Echocardiography was performed and reported as normal. He was then referred to the neurosurgery ward and was hospitalized for almost 40 days.
He had no signs and symptoms related to COVID-19. However, during hospitalization, spiral high-resolution computed tomography (HRCT) scan of his lung without contrast revealed patchy ground-glass opacity in both lungs (mostly in the right lung) (Fig. 1). These findings suggested that the patient was infected by COVID-19. Finally, the COVID-19 infection was confirmed by consecutive positive reverse transcription polymerase chain reaction (RT-PCR) test.
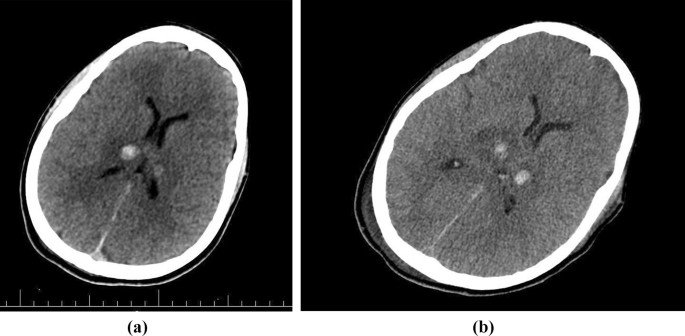
Following a brain CT scan, a deep intracranial hemorrhage in the thalamus was found (Fig. 2A). The contusion of the right parietal lobe without hydrocephalus and midline shifts were reported (Fig. 2B). Furthermore, no spinal fractures and displacements were reported in his cervical spine CT scan. Abdominal and pelvic CT scan were also normal.
His laceration of the parietal region was repaired by surgery. In addition, the repair and debridement of the right knee laceration were carried out. Afterward, he was intubated and a collar fixed his cervical spine. He was treated with lasix and mannitol because of raised intracranial pressure. After supportive therapy for almost 40 days, he was discharged after educating his parents about his care at home, while his GCS was 6/15 (E2V1M3).
Discussion
In this study, we reported a 14-year-old boy referred to the ER due to multiple trauma. He had no history of coagulopathy or anticoagulant consumption. In this case, trauma precipitated parietal contusion. Through medical interventions, bilateral basal ganglia hemorrhage was discovered incidentally.
Several clinical reports and series exploring the relationship between COVID-19 and ischemic strokes have been published [5].
Neurologic symptoms in COVID-19 can be divided into several categories, ranging from nonspecific symptoms such as a headache to severe forms such as cerebrovascular disease [6].
Basal ganglia hemorrhage due to traumatic events is rare [7].
Systemic and metabolic disease, neurodegenerative disease, and vascular disease can involve basal ganglia and thalamus [8, 9].
COVID-19, like other acute respiratory syndromes, can invade the central nervous system (CNS) through hematogenous and neuronal dissemination, or it can be an immune response to the cytokine storm [10, 11].
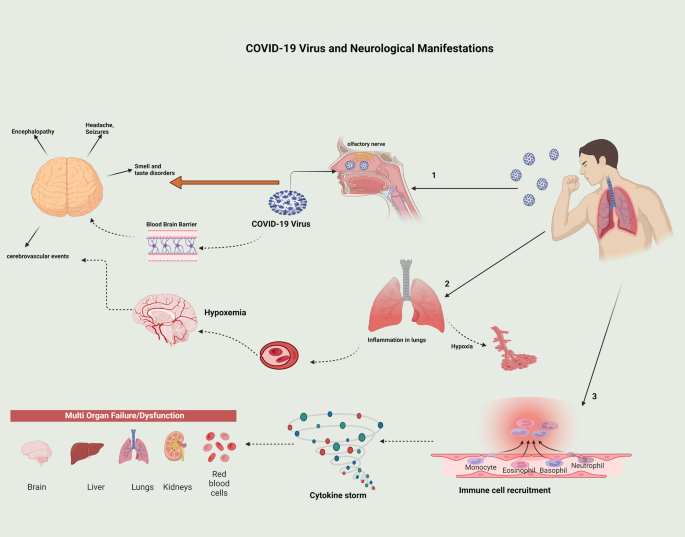
There is not enough data about the underlying mechanisms of neurological disorders caused by COVID-19. A total of 2% of patients have neurological symptoms. One of the ways in which COVID-19 can invade the neurological system is through the mucous layer of the nose that contains the olfactory receptor cells. Olfactory nerves might deliver viruses and infections to the brain. On the other hand, COVID-19 causes respiratory infection and the level of oxygen in blood may decrease. Brain function can be impaired through hypoxemia (Fig. 3) [12].
Some other pathophysiology of ischemic stroke in COVID-19 are hypoperfusion of the brain, hypertension leading to posterior reversible encephalopathy syndrome, and septic embolization in patients with bacterial superinfection (Fig. 3) [13].
ACE2 serves important roles in various parts of the body, such as the lung, kidney, brain, liver, and endothelial cells. COVID-19 decreases the expression of ACE2. Due to reduced ACE2 levels, the renin–angiotensin–aldosterone system (RAAS) will deteriorate and cause multiorgan damage. Diminished ACE2 can cause intracerebral hemorrhage through several mechanisms. For instance, increasing the blood pressure, endothelial dysfunction, damage to the brain vessels, and finally depression of angiotensin-(1-7) and Mas receptor [Ang (1-7)/MasR] signaling, which has a neuroprotective, antifibrotic, and vasodilatory effect [14, 15].
Immune response to the cytokine storm and chemokines can disrupt the blood–brain barrier and neuroinflammation. The breakdown of the blood–brain barrier and inflammation both have a main role in ischemic stroke [16, 17].
Intracranial hemorrhage was documented in some cases as a complication of COVID-19. Some risk factors are arterial hypertension and anticoagulation therapy (pretreatment of unrelated disease to COVID-19 thromboprophylaxis) [2].
Hyperinflammatory state may be the main cause of complication in patients with diabetes mellitus (DM) as well as COVID-19. A case series was reported in October 2020 that included three patients with COVID-19 and ICH. All three patients had risk factors for ICH such as hypertension and DM. DM and ICH are associated through some mechanisms. High blood glucose can cause endothelial dysfunction. Dysfunction of the brain’s small vessel endothelial can lead to ICH [14].
There is a hypothesis that the state of hyperinflammation in diabetic patients is related to higher mortality in these patients [18]. High C-reactive protein (CRP) levels are a risk factor for stroke. High CRP levels may lead to ICH in patients with COVID-19 [19].
We reported a 14-year-old boy with bilateral basal ganglia hemorrhage and documented COVID-19. Our patient had no special past medical history of hypertension, DM, and other diseases. There is no evidence that he consumed anticoagulant agents before. There is some research that ICH is propounded as a complication of COVID-19. Basal ganglia hemorrhage related to trauma is rare [7].
The underlying pathophysiology for COVID-19 related ICH can involve hyperinflammatory state due to increased cytokine production. Although a few case series and case reports were published on some patients COVID-19 as well as ICH, more investigation and research regarding the association between COVID-19 and ICH are needed.
Conclusions
It is essential to discover the pathophysiology of neurological manifestations of COVID-19. Neurological findings of COVID-19 range from mild conditions such as headache to severe conditions such as stroke. Therefore, acknowledgement as to the causes and prevention of the situations leading to critical events should be considered in treatments of COVID-19.
Availability of data and materials
The datasets obtained and analyzed in the current study are available from the corresponding author upon reasonable request.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- CT scan:
-
Computed tomography scan
- ICH:
-
Intracranial hemorrhage
- GCS:
-
Glasgow Coma Scale
- ECG:
-
Electrocardiogram
- RT-PCR:
-
Reverse transcription polymerase chain reaction
- CNS:
-
Central nervous system
- DM:
-
Diabetes mellitus
- CRP:
-
C-reactive protein
- ER:
-
Emergency room
- ARDS:
-
Acute respiratory distress syndrome
- ACE2:
-
Angiotensin-converting enzyme 2
- HRCT:
-
High-resolution CT scan
- RAAS:
-
Renin–angiotensin–aldosterone system
- Ang(1-7)/MasR:
-
Angiotensin-(1-7) and Mas receptor
References
Wu F, Zhao S, Yu B, Chen Y-M, Wang W, Song Z-G, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–9.
Margos NP, Meintanopoulos AS, Filioglou D, Ellul J. Intracerebral hemorrhage in COVID-19: a narrative review. J Clin Neurosci. 2021;89:271–8.
Sharifi-Razavi A, Sedaghat Z, Baziboroun M, Karimi N. COVID-19 accompanied with intracerebral hemorrhage: a case series. Arch Clin Infect Dis. 2020;15(4): e104877.
Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host–virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci. 2020;11(7):995–8.
Benger M, Williams O, Siddiqui J, Sztriha L. Intracerebral haemorrhage and COVID-19: clinical characteristics from a case series. Brain Behav Immun. 2020;88:940.
Abboud H, Abboud FZ, Kharbouch H, Arkha Y, El Abbadi N, El Ouahabi A. COVID-19 and SARS-Cov-2 infection: pathophysiology and clinical effects on the nervous system. World Neurosurg. 2020;140:49–53.
Kankane VK, Gupta TK, Jaiswal G. Traumatic bilateral basal ganglia bleed: a report of rare two cases and review of the literature. Asian J Neurosurg. 2016;11(4):457.
Ghoshal S, Gokhale S, Rebovich G, Caplan LR. The neurology of decreased activity: abulia. Rev Neurol Dis. 2011;8(3–4):e55-67.
Bao Y, Lin SY, Cheng ZH, Xia J, Sun YP, Zhao Q, et al. Clinical features of COVID-19 in a young man with massive cerebral hemorrhage—case report. SN Compr Clin Med. 2020;2(6):703–9.
Haddadi K, Ghasemian R, Shafizad M. Basal ganglia involvement and altered mental status: a unique neurological manifestation of coronavirus disease 2019. Cureus. 2020;12(4): e7869.
Alqahtani A, Alaklabi A, Kristjansson S, Alharthi H, Alam H. Acute necrotic hemorrhagic leukoencephalitis related to COVID-19: a report of 2 cases. Radiol Case Rep. 2021;16(9):2393–8.
Ahmadirad N, Ghasemi Z. COVID-19 and central nervous system: entry routes and. Basic Clin Neurosci. 2020;11(2):217.
Yaghi S, Ishida K, Torres J, Mac Grory B, Raz E, Humbert K, et al. SARS-CoV-2 and stroke in a New York healthcare system. Stroke. 2020;51(7):2002–11.
Pavlov V, Beylerli O, Gareev I, Torres Solis LF, Solís Herrera A, Aliev G. COVID-19-related intracerebral hemorrhage. Front Aging Neurosci. 2020;12:352.
Steardo L, Steardo L Jr, Zorec R, Verkhratsky A. Neuroinfection may contribute to pathophysiology and clinical manifestations of COVID-19. Acta Physiol. 2020;229: e13473.
Liu R, Pan M-X, Tang J-C, Zhang Y, Liao H-B, Zhuang Y, et al. Role of neuroinflammation in ischemic stroke. Neuroimmunol Neuroinflamm. 2017;4:158–66.
Yang C, Hawkins KE, Doré S, Candelario-Jalil E. Neuroinflammatory mechanisms of blood–brain barrier damage in ischemic stroke. Am J Physiol Cell Physiol. 2019;316(2):C135–53.
Tadic M, Cuspidi C, Sala C. COVID-19 and diabetes: is there enough evidence? J Clin Hypertens. 2020;22(6):943–8.
Liu Y, Wang J, Zhang L, Wang C, Wu J, Zhou Y, et al. Relationship between C-reactive protein and stroke: a large prospective community based study. PLoS ONE. 2014;9(9): e107017.
Acknowledgements
The author would like to thank Parnian Shobeiri for commenting on this manuscript.
Funding
This research did not receive any specific grant from funding agencies.
Author information
Authors and Affiliations
Contributions
PA, NN, and MZ treated the patient. SM and PA wrote the manuscript. All authors revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institutional board review at Guilan University of Medical Sciences with the ethics code of IR.GUMS.1401.276.
Consent for publication
Written informed consent was obtained from the patient’s legal guardian for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Asadi, P., Maleki, S., Zia Ziabari, S.M. et al. A 14-year-old boy with multiple trauma and bilateral basal ganglia hemorrhage due to coronavirus disease 2019: a case report. J Med Case Reports 17, 88 (2023). https://doi.org/10.1186/s13256-023-03824-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-023-03824-1