- Case report
- Open access
- Published:
Kernicterus by glucose-6-phosphate dehydrogenase deficiency: a case report and review of the literature
Journal of Medical Case Reports volume 2, Article number: 146 (2008)
Abstract
Introduction
Glucose-6-phosphate dehydrogenase deficiency is an X-linked recessive disease that causes acute or chronic hemolytic anemia and potentially leads to severe jaundice in response to oxidative agents. This deficiency is the most common human innate error of metabolism, affecting more than 400 million people worldwide.
Case presentation
Here, we present the first documented case of kernicterus in Panama, in a glucose-6-phosphate dehydrogenase-deficient newborn clothed in naphthalene-impregnated garments, resulting in reduced psychomotor development, neurosensory hypoacousia, absence of speech and poor reflex of the pupil to light.
Conclusion
Mutational analysis revealed the glucose-6-phosphate dehydrogenase Mediterranean polymorphic variant, which explained the development of kernicterus after exposition of naphthalene. As the use of naphthalene in stored clothes is a common practice, glucose-6-phosphate dehydrogenase testing in neonatal screening could prevent severe clinical consequences.
Introduction
Glucose-6-phosphate dehydrogenase (G6PD) is a housekeeping enzyme that catalyzes the first step in the pentose phosphate pathway, providing reducing power in the form of nicotinamide adenosine dinucleotide phosphate (NADPH). This metabolic pathway is the only source of NADPH in erythrocytes and is therefore the mechanism by which the cell damage caused by oxidative stress is avoided [1, 2].
Individuals deficient in G6PD are usually asymptomatic; however, in some cases exposure to chemicals (for example, naphthalene) and drugs (including sulfamides, antipyretics, nitrofurane, primaquine and chloroquine) can induce massive intravascular hemolysis. Among the clinical forms of this enzymatic deficiency are jaundice, acute hemolytic anemia and chronic nonspherocytic hemolytic anemia. A more severe consequence of neonatal hyperbilirubinemia is kernicterus, a neurological syndrome caused by the deposition of bilirubin in the brain tissues, which results in severe consequences and even death [2–4].
G6PD deficiency is an X-linked recessive disease and is the most common human innate error of metabolism, affecting more than 400 million people worldwide [5]. The G6PD gene is highly polymorphic and more than 140 mutations have been described. In the Mediterranean, Middle East, India, China and Southeast Asia, the distribution of multiple alleles account for the total prevalence. There are no reports concerning the prevalence of this enzymatic deficiency in Panama; however, our preliminary studies indicate a high prevalence of G6PD deficiency in this country (unpublished data).
Here we present a kernicterus case in a G6PD-deficient newborn resulting in severe neurological damage.
Case presentation
Clinical history
A 4-day-old boy was admitted to the Hospital del Niño in Panama. He was the first child of a healthy young woman from a normal vaginal birth at term. He had an Apgar score of 9 at 1 minute and 9 at 5 minutes, a birth weight of 3.5 kg, body length of 53 cm and a 35 cm cephalic circumference. The newborn was hospitalized when clinical examination revealed 4+ jaundice, hypoactivity, hyporexia and generalized tonic-clonic seizures, requiring management with anticonvulsives, phototherapy and exchange transfusion. A history of use of naphthalene-impregnated clothes was recorded. Analysis of clinical symptoms and laboratory tests diagnosed the proband with kernicterus by G6PD deficiency. Despite clinical management, after 5 years the patient presented with reduced psychomotor development, neurosensory hypoacousia, absence of speech and poor reflex of the pupil to light.
Laboratory data
Upon admission the patient presented total bilirubin values of 42.6 mg/dl (41.8 mg/dl from indirect bilirubin), 11.8 g/dl hemoglobin, 8% reticulocytes, O (Rh+) and B (Rh+) blood types for child and mother, respectively, and negative direct Coombs. G6PD testing was reported as deficient, and the quantification of the serum levels of this enzyme was 0.278 U/gHb (normal value range 4.6 to 13.5 U/gHb). Cranial magnetic resonance imaging demonstrated hyperintense basal ganglia lesions on T2-weighted images (Figure 1).
Mutational analysis
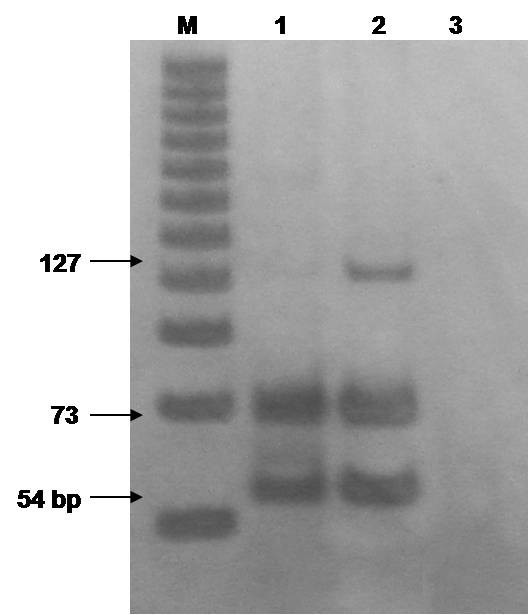
Determination of the G6PD polymorphic variant was achieved by polymerase chain reaction and restriction fragment length polymorphism (PCR-RFLP) as described elsewhere [6]. Genomic DNA from the patient and one heterozygote G6PD Mediterranean variant control were obtained from heparinized peripheral blood with the salting out method described by Miller et al. [7]. We used 100 ng of DNA to amplify the region flanking nucleotide 563 containing the polymorphism. Amplified products were then digested with the restriction enzyme Mbo II and the digestion mix was electrophoresed in 10% polyacrylamide gel. Analysis showed the G6PD Mediterranean polymorphic variant genotype (Figure 2), which explained the G6PD deficiency phenotype.
Conclusion
G6PD deficiency is an X-linked recessive disease and is the most common human innate error of metabolism, affecting more than 400 million people worldwide [5]. At the Hospital del Niño of Panama, we have observed a high prevalence of G6PD deficiency in our patients; however, there are no reports concerning the prevalence of this enzymatic deficiency in this country.
Here we presented the first documented case of kernicterus in Panama in a G6PD-deficient newborn. The proband presented with hyperbilirubinemia (total bilirubin of 42.6 mg/dl) and was treated with phototherapy and two exchange transfusions. G6PD deficiency testing was positive explaining the symptoms and clinical signs. Mutational analysis demonstrated the G6PD Mediterranean polymorphic variant genotype (Figure 2).
The use of naphthalene-impregnated clothes prior to the episodes of seizure explained the development of severe jaundice that led to kernicterus. As the use of naphthalene in stored clothes is a common practice, so testing for G6PD as part of neonatal screening could prevent this severe clinical consequence.
Consent
Written informed consent was obtained from the patient's next-of-kin for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
Beutler E: G6PD deficiency. Blood. 1994, 84: 3613-3636.
Luzzatto L, Mehta A, Vulliamy T: Glucose-6-phosphate dehydrogenase deficiency. The Metabolic and Molecular Basis of Inherited Disease. Edited by: Scriver ChR, Beaudet AL, Sly WS, Valle D. 2001, New York: McGraw Hill, 4517-4553. 8
Beutler E: Study of glucose-6-phosphate dehydrogenase: history and molecular biology. Am J Hematol. 1993, 42: 53-58. 10.1002/ajh.2830420111.
Kaplan M, Beutler E, Ureman HJ, Hammerman C, Levi-Lahad E, Renbaum P, Stevenson DK: Neonatal hiperbilirubinemia in glucose-6-phosphate dehydrogenase deficient heterozygotes. Pediatrics. 1999, 104: 68-74. 10.1542/peds.104.1.68.
Luzzatto L: Glucose-6-phosphate dehydrogenase deficiency: from genotype to phenotype. Haematologica. 2006, 91: 1303-1306.
Vaca G, Arambula E, Monsalvo A, Medina C, Nunez C, Sandoval L, Lopez-Guido B: Glucose-6-phosphate dehydrogenase (G-6-PD) mutations in Mexico: four new G-6-PD variants. Blood Cells Mol Dis. 2003, 31: 112-120. 10.1016/S1079-9796(03)00119-0.
Miller SA, Dykes DD, Polesky HF: A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 1988, 16: 1215-10.1093/nar/16.3.1215.
Acknowledgements
EAM, RRP and MAM are SNI fellows. This work was supported by the General Coordination of Research and Postgraduate (CGIP-PROFAPI) Universidad Autónoma de Sinaloa and CECYT (State Council of Science and Technology) from Sinaloa, México.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
GCG provided genetic counseling to the parents. JJA and ED collected the data. MAM, EAM and GVP conducted the data analysis, interpreted experiments and revised the manuscript. MAM, RRP, NGM and EAM performed genetic studies and elaboration, and helped to draft the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Cossio de Gurrola, G., Araúz, J.J., Durán, E. et al. Kernicterus by glucose-6-phosphate dehydrogenase deficiency: a case report and review of the literature. J Med Case Reports 2, 146 (2008). https://doi.org/10.1186/1752-1947-2-146
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1752-1947-2-146